Talk:Reference ranges for blood tests/Archive 1
| This page is an archive of past discussions. Do not edit the contents of this page. If you wish to start a new discussion or revive an old one, please do so on the current talk page. |
UK Ranges
I'm puzzled by the number of analytes that have "UK ranges" in brackets e.g. 'Sodium: 130 - 145 mmol/L (UK 135-146 mmol/L)'. Surely the UK is not biochemically different to the rest of the world? Indeed it has as much of a racial mix as continental Europe or the USA. I'm assuming that the two different ranges came from two different textbooks, one of which happens to be published in the UK. I think some consensus should be reached for these analytes, and a single range quoted (NB age-, sex- and pregnancy-related ranges really will be different!). Scolaire 15:17, 12 July 2006 (UTC)
I have recently moved to the US from the UK, and strangely enough all recommendations as to reference ranges and even the doses of drugs are different. So I don't think it would be appropriate to just convert values. Actually the reason for this post is that in the US, the reference ranges for serum lipids are in mg/dL. These seem to be in the articles linked from this section, but not here. Jkwan 12:19, 23 October 2006 (UTC)
I have no problem with the difference between SI units and "American" units. What bugs me is a range such as "2.6 - 6.8 mmol/L or 10 - 20 mg/dL (UK 2.5 - 6.4 mmol/L)". Now, you can say "UK 2.5 - 6.4 mmol/L, US 10 - 20 mg/dL" — that makes perfect sense; but to say that a urea of 6.5 mmol/L is normal for anybody in the US and raised for anybody in the UK is bizarre! What's needed for all of these analytes is two sets of agreed reference ranges only - one in SI units and one in "American" units. I may get around to doing it myself some day but I'm kinda hoping somebody else will do it first. Scolaire 20:38, 23 October 2006 (UTC)
Regardless of whether or not the actual normal ranges for these tests in the populations of the UK and US are the same, doctors in the two countries use different values. This may result from the fact that different proffesional bodies in the two countries come up with different recommendations using different sources. I think it is right to quote both - so that patients can see the reference values their doctor uses to make decisions. Incidently, within the UK different NHS hospitals use slightly different reference ranges (for example some hospitals take the upper limit for potassium to be 5.5). Jkwan 19:01, 9 November 2006 (UTC)
Jkwan, you're missing the point - hospital laboratories everywhere use slightly different reference ranges for everything. These may be derived in-house, taken from a textbook or taken from an instrument manual. There is no standard set of ranges for anything anywhere. That is precisely why they are called reference ranges, not absolute ranges or some such. You may as well say "All Saints: 2.6-6.8, St. Elsewhere's: 2.5-6.4" as say "US: 2.6-6.8, UK: 2.5-6.4". There is no national difference between ranges for any of the analytes in this article. The manual for an American analyser (say, Abbott) or a European analyser (say, Roche) will quote the same ranges in America as in Europe, and labs using that analyser will quote those ranges wherever in the world they are. Hospitals using textbooks are just as likely to use Tietz in Europe as in America. What you are saying is that you were accustomed to one set of ranges when you were in the US, and then met a different set of ranges when you went to Britain, but had you walked half a mile down the road you would probably have seen just as big a difference. Patients reading this article will not see the reference values their doctor uses to make decisions, only the particular one (or in this case two) that a particular editor encountered in a particular lab. In the end, it doesn't matter which one we go with — they are all roughly the same and they are only for reference anyway — but there needs to be only one set! Scolaire 21:59, 9 November 2006 (UTC)
Readability
May I suggest separating the reference ranges and the units used into separate columns. Right now, I'm having trouble with readability. If I already know a test number and unit of measure, all I'm after is the high/low range. That's hard to see with the current setup. Also, I would love to see headers for each column.
I'm willing to do the actual grunt work to fix this, but I didn't want to just go muck in someone else's entry.
dafydd 05:44, 27 December 2006 (UTC)
Urinalysis
Any opinion on whether it would be a good idea to include the reference ranges for Urinalysis? Standard values are not listed on the urinalysis wiki. If I don't hear from anyone within a week or so I'll add it in. --Robb37 06:01, 18 April 2007 (UTC)
- Provisional no. Firstly the article title is "Reference ranges for common blood tests", so urine testing would be excluded. Secondly the "common" tests on urine are those of dip-testing for blood, sugar and protein in a clinic setting (for which a normal value would be "negative"); whereas quantative tests done in a laboratory (eg calcium, oxalate) are relatively infrequently requested.
- I'm not sure which tests you have in mind, but they might be better under a new article, perhaps titled Reference ranges for urine tests. David Ruben Talk 13:14, 18 April 2007 (UTC)
- Might need make reference/links from Urine and Human urine to this information page :-) David Ruben Talk 13:24, 18 April 2007 (UTC)
- True enough. I found this page as a redirect from Normal lab values so I didn't notice the blood qualifier in the article title. While I don't necessarily think that the inclusion of pH, Osmolarity, Specific gravity, etc. would detract from the article, I agree that this would be outside the scope of the article as currently titled. --Robb37 01:29, 19 April 2007 (UTC)
Recent edits
I'm not happy in general with the recent edits — the tables have been pulled out of shape, the most common tests, i.e. U&E, have been brought down while tumour markers have been brought to the top, and the "Biochemistry" heading has been unjustifiably removed. But let me start with this question: what on earth is meant by "osmolarity: LL <300, UL >300"? Why not just say "LL zero, UL infinity"? Scolaire (talk) 17:37, 2 January 2008 (UTC)
Not having had an answer even to that I have reverted as follows:
- "Clinical Biochemistry" is the name of the discipline - it doesn't mean that haematology isn't clinical
- de-linked CHEM-7 and CHEM-20: no articles actually exist
- "Acid base physiologys" => "Acid base physiology" and moved it to after electrolytes
- reverted to original format (most common analytes first)
- put phosphate with calcium, where it belongs
- put chloride with sodium and potassium, where it belongs
- osmolarity => osmolality and enter proper ref. range from Tietz
- and maybe more - it's a lot of editing in one go.
Scolaire (talk) 23:07, 25 January 2008 (UTC)
I made some edits to this article [1], which, however, need to be discussed before inclusion:
- Split of clinical biochemistry into smaller sections. As per Section size policies I really consider this hard knowledge, and thus it justifies being split into smaller sections. As it is now it is very hard to do any further contributions. Enabling further section-editing would facilitate this.
- Addition of iron-related values, since they are clinically important.
Mikael Häggström (talk) 06:38, 17 February 2008 (UTC)
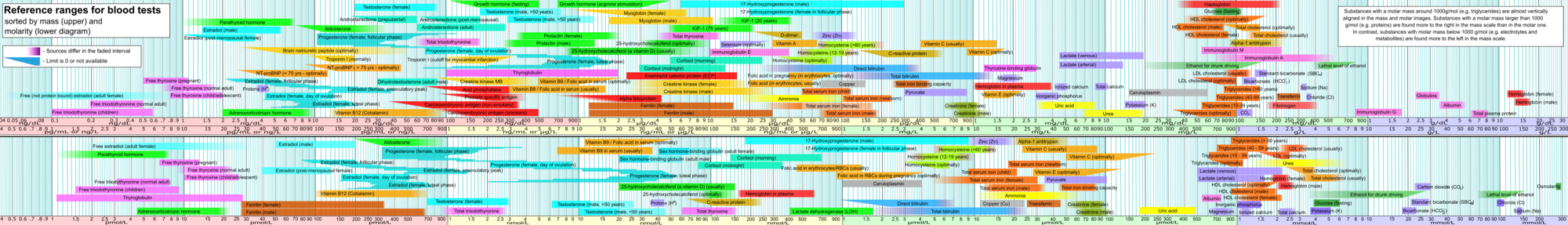
Sorted by concentration
There, more easy to overview, and more colorful too. Feel free to correct it, or leave me a note if you find it incorrect. Mikael Häggström (talk) 07:19, 26 October 2008 (UTC)
Svg blurry
I replaced the first one with the vector file, since it will likely be edited many many times. However, does anybody know how to avoid making it appear blurry as it does now? In Inkscape it is as sharp as the png one. Mikael Häggström (talk) 20:23, 30 October 2008 (UTC)
Glucose levels
Fasted glucose levels, the upper limit for these is internationally defined by the WHO, as per values shown at Glucose tolerance test. Not quite sure how table range-limiting being done, but limit for normal fasting is under 6.1 (hence "<6.1" or "<100" in US used units).
Previous 5.8-6.1 (105-110) is wrong both ways: a) internationally 5.9 is still "normal" and not impaired fasting glycemia (IFG) and (b) that 6.1 itself is nolonger normal but does constitute IFG if repeatable (but 6.09 is just normal). David Ruben Talk 15:02, 10 November 2008 (UTC)
My edits
To summarize the edits I've made recently, so you may not have to go through them all:
- Added missing values mentioned in that Bloodbook.
- Added references to some molar values.
- Removed some values where references were missing, because they may not be that essential if they were not mentioned in any of these sources.
Mikael Häggström (talk) 08:18, 28 November 2008 (UTC)
Plasma or total blood concentration?
I'm actually not 100% sure on this point: For a plasma concentration, is it the concentration compared to 1 L or dL of plasma or 1 L or dL of blood (including cells)? Mikael Häggström (talk) 16:03, 30 December 2008 (UTC)
Nutrition manufacturer as reference
I took some optimal ranges from the nutrition manufacturer Adëeva, although there might be a bias, giving higher recommended values than necessary. Still, their reference list seems reliable, and I took examples where there probably is a good reason to keep levels in that optimal range. Mikael Häggström (talk) 08:56, 9 July 2009 (UTC)
Cortisol
Please add the values for cortisol. Best regards, --CopperKettle 09:55, 25 October 2009 (UTC)
Parathyroid hormone (PTH)
Where did PTH go...? /Stage —Preceding unsigned comment added by 130.226.172.129 (talk) 09:11, 7 December 2009 (UTC)
- Actually, PTH has never been here. Mikael Häggström (talk) 10:34, 7 December 2009 (UTC)
Troponin Reference Ranges
I was asked to change the previous troponin info by a Consultant Biochemist who felt the info was dangerously misleading as it is not a simple range. Mikael Häggström was after a citation but its not quite that simple. Ranges are assay dependent but this paper provides definitive cut offs for the calculation of MI and ACS by troponin. http://eurheartj.oxfordjournals.org/cgi/reprint/28/20/2525.pdf Could you insert the ref to the article Mikael as I don't usually contribute to scientific pages and not fully up on correct ref method
Cheers andrewdpcotton
- Sure I can do that. I agree that more specific troponin values were needed. Sorry to be picky, however, but I didn't find those numbers in that European Heart Journal article either. It is very useful for describing troponin generally in the troponin article, but it should provide a way to confirm what is added in Wikipedia. Mikael Häggström (talk) 06:26, 15 December 2009 (UTC)
Hi Mikael, Unfortunately Clinical Biochemistry is a little more complicated than just listing numbers. The article provides the method by which the ranges may be calculated to the 99th percentile. The actual ranges used are then dependent on the specific assay and equipment used. This varies by manufacturer and local practice but will produce ranges similar to those shown. These ones for example are those used by South London Healthcare NHS Trust.
For example see Table 2 in this article to see how Troponin ranges vary by manufacturer http://www.clinchem.org/cgi/reprint/49/8/1331. Note however that this article predates the 2007 one so the values have changed slightly since then and the definition split between ACS and MI is not given in this article (Note also that the Roche figure is for Troponin-T and all other manufacturers are for Troponin-I). I have asked my biochemistry sources if there is a definitive online citation with current ranges available but at present it seems that it is currently something defined by individual Biochemistry units. Ranges used will be in this region though as can be seen from the 2003 article.
If anything more straightforward appears I'll let you know but I'm afraid this will have to do for now. Its certainly more accurate than what you had before on the article. Andrewdpcotton (talk) 10:35, 15 December 2009 (UTC)
- Indeed, they are more specific than the previous value. I gave South London Healthcare NHS Trust as reference. Surely, a more specific one would be preferable, for example with an URL link, but it's better than nothing. Mikael Häggström (talk) 16:51, 15 December 2009 (UTC)
Testosterone
The level listed in this article seems to conflict with the article Hypogonadism. Can someone experienced in the matter reconcile the contradiction? Thanks, Vectro (talk) 19:10, 31 December 2009 (UTC)
- The values there seem to lie within the normal variability among sources. Mikael Häggström (talk) 08:48, 4 January 2010 (UTC)
Zinc serum reference range changed
I have changed the Zinc serum reference range. It is very difficult to find Zinc reference range values online. I just had a blood test with Zinc reference range of 70-150 ug/dL I was able to find an online reference at: http://www.dlolab.com/PDFs/DLO-OCTOBER-2008-LAB-UPDATE.pdf Its shows a reference range of 60-130 ug/dL. Gordon55y (talk) 01:02, 17 January 2010 (UTC)
- Good job. Thanks Mikael Häggström (talk) 05:22, 17 January 2010 (UTC)
No need to split because of size in KB
This article is now more than 60KB as shown in edit mode. However, most of the size of the article lies in table code and footnotes. When copying the readable prose when not in edit mode, it was only 15KB in a txt document, classifying it as Length alone does not justify division in Wikipedia:Splitting. Mikael Häggström (talk) 10:04, 6 December 2009 (UTC)
- On second thought, I'm actually not sure anymore whether to split or not. Mikael Häggström (talk) 16:27, 22 April 2010 (UTC)
Dubious ALT value
The following value for ALT, 1, taken from MERCK MANUALS, deviates very much from the rest. I think there needs to be additional confirmation before it could be reinserted. Mikael Häggström (talk) 12:10, 29 April 2010 (UTC)
Splitting
The problem with splitting this article is that there are so many sections, so if each one would be forked away to a separate article, then there would be so many articles that it would be very hard to find individual values. Now, they can easily be found by the search functions of browsers, but that ability would be lost in a split. Mikael Häggström (talk) 19:28, 29 April 2010 (UTC)
Copper
Copper appears twice in the table, with the same range. —Preceding unsigned comment added by 87.69.218.34 (talk) 16:35, 21 May 2010 (UTC)
C-reactive protein (CRP)
C-reactive protein (CRP) values are not aligned with the table. It means that the units are displayed under the "Upper limit" culomn. —Preceding unsigned comment added by 87.69.218.34 (talk) 16:53, 21 May 2010 (UTC)
C-reactive protein (CRP)
C-reactive protein (CRP) appears twice in different sections. —Preceding unsigned comment added by 87.69.218.34 (talk) 16:56, 21 May 2010 (UTC)
- How perceptive. It's fixed now. Mikael Häggström (talk) 17:18, 21 May 2010 (UTC)
Ketones: acetoacetate and beta-hydroxybutyrate
Can someone add the reference ranges for these? —Preceding unsigned comment added by 174.53.65.175 (talk) 16:39, 28 May 2010 (UTC)
Someone to complete searchable HTML version
It would be much more useful with a diagram with searchable substance names. There is a version of Blood values sorted by mass and molar concentration with blank boxes for availing translation or usage of HTML/CSS code to make the substance names searchable in a web browser.
An incomplete version is found on this external page (great thanks to Peter A. Ensminger). It would be very appreciated if someone with knowledge in HTML could complete the page. Mikael Häggström (talk) 17:01, 28 May 2010 (UTC)
One much-cited authority seems to be a piracy, malware, phishing, and scamming site
This rcpa manual section seems a most-useful and much cited source: E.g., "Royal College of Pathologists of Australasia; Cholesterol (HDL and LDL) - plasma or serum" http://www.rcpamanual.edu.au/sections/pathologytest.asp?s=33&i=450
"The on-line RCPA Manual ... pre-eminent source of pathology information for health care practitioners and as a valuable companion for the consumer resource Lab Tests Online ... " (LTOAU http://www.labtestsonline.org.au/) (No apparent malware, 2010 Nov 4)
However, RCPA Manual seems to be on a web page that is used to distribute malware, e.g., "Distributes trojans, driveby downloads and other malware. ... " Phishing ... scamming ... http://www.mywot.com/en/scorecard/rcpamanual.edu.au
Here's another report of multiple exploits on the site: http://support.clean-mx.de/clean-mx/viruses.php?domain=rcpamanual.edu.au&sort=first%20desc
Perhaps a better site can be found hosting the RCPA Manual? That was the only site I saw in a quick look.
Perhaps someone could politely notify the rcpamanual.edu.au that their website has been pwned by scammers? The cite for the Royal College of Pathologists of Australasia (RCPA) is www.rcpa.edu.au
Wikipedia shouldn't offer links designed to leave readers at the mercy of known scamming, malware, or phishing sites. I suggest the reference be taken down. —Preceding unsigned comment added by 68.165.11.149 (talk) 01:34, 5 November 2010 (UTC)
File:Blood values sorted by mass and molar concentration.png to appear as POTD soon
Hello! This is a note to let the editors of this article know that File:Blood values sorted by mass and molar concentration.png will be appearing as picture of the day on March 26, 2011. You can view and edit the POTD blurb at Template:POTD/2011-03-25. If this article needs any attention or maintenance, it would be preferable if that could be done before its appearance on the Main Page so Wikipedia doesn't look bad. :) Thanks! howcheng {chat} 18:14, 24 March 2011 (UTC)
- A good choice of POTD
 Mikael Häggström (talk) 18:00, 11 April 2011 (UTC)
Mikael Häggström (talk) 18:00, 11 April 2011 (UTC)
I support this. Mikael Häggström (talk) 15:07, 19 August 2012 (UTC)
- Why? Both of these articles are huge, they do not have overlapping content, nothing in either of them should be deleted, and if they were merged it would make two huge articles even more humongous. Blue Rasberry (talk) 18:47, 30 August 2012 (UTC)
Healthy ranges vs Normal (average) ranges
It is sad that there is no mention in the article or here in the Talk about healthy ranges, as distinguished from average ranges.
Why would I want my numbers compared to a range that was derived from from people who are deficient in vitamin D, who smoke, who are overweight, who have insulin resistance, who are sleep deprived, who are diagnosed with chronic disease, who drink more than a little occasionally, who are on drugs of any kind, etc.?
Encyclopedant (talk) 07:07, 20 May 2013 (UTC)
- Indeed, it would be good to have a column giving "therapeutic targets" or "optimal ranges" for all tables in the article, such as in the Lipids or Vitamins sections. The problem is, such values are not available for all blood components, or no Wikipedia editor has found those studies. Feel free to add such values if you find any out there. Mikael Häggström (talk) 19:52, 20 May 2013 (UTC)
References on hemoglobin in mmol/L
The reference values for hemoglobin in mmol/L are absolutely incorrect. Please delete the references 131 and 132. This paper does not give reference values for Hb. Can somebody come up with a better source for Hb reference values? Prof R Wevers, Nijmegen (author of 131 and 132)
- This reference was not used for the actual reference range, but merely the molar mass of hemoglobin in order to convert from mass concentrations. I've clarified this point in the references now. Mikael Häggström (talk) 14:39, 29 December 2012 (UTC)
No, the values are absolute rubbish. The correct values in mmol/L are 8,7 - 11,2 for men, and 7,5 - 9,9 for women, see German page for hemoglobin. The has to be changed, pronto. — Preceding unsigned comment added by 37.247.74.50 (talk) 11:27, 31 July 2013 (UTC)
- I see no reference for the values on the German page for hemoglobin. Another Wikipedia page is not a reliable source for this page, so you need to find one for this claim to justify a change in the article. Mikael Häggström (talk) 16:54, 31 July 2013 (UTC)
This is incredible. It is so wrong it could cost a patient their life, if any doctor were foolish enough to trust the value listed here in mmol/L ...since the patient would be long dead before such a concentration could ever be reached. Reference? Any medical book you hold in your hand that uses the SI units (mmol/L). http://www.etoolsage.com/Calculator/Hemoglobin_Calculator.asp . Just fix it immediately, a Professor has mentioned it (above), and I'm a physician, our lab uses mmol/L and the reference ranges written in the previous comment. — Preceding unsigned comment added by 37.247.74.50 (talk) 11:08, 1 August 2013 (UTC)
- The values you state are not hemoglobin but hemoglobin subunits, which are calculated by multiplying the hemoglobin values by 4. A more detailed explanation is given in:
- Lodemann, P.; Schorer, G.; Frey, B. M. (2009). "Wrong molar hemoglobin reference values—a longstanding error that should be corrected". Annals of Hematology. 89 (2): 209. doi:10.1007/s00277-009-0791-x. PMID 19609525.
- I've added the Hb subunits values in the article as well for clarity. Mikael Häggström (talk) 20:11, 1 August 2013 (UTC)
Ok, better, but still suboptimal, since, when talking about Hb in any clinical context, either g/L, mg/dL, or mmol/L is used, and when mmol/L is used, perhaps "technically" the subunits of hemoglobin are being reffered to, but that is the measure, and it is simply called Hb in the lab reports, not "Hb subunits". So I propose you use the Hb subunits mMol in place of the confusing "complete" Hb you reference, and add a note that the subunits are referred to as is usual in a clinical context(to please the biochemists). — Preceding unsigned comment added by 37.247.74.50 (talk) 09:20, 2 August 2013 (UTC)
- I've noted that "hemoglobin subunits" can sometimes be displayed as simply "hemoglobin", but I don't think it should be encouraged to use the subunit value by default. Mikael Häggström (talk) 09:11, 3 August 2013 (UTC)
UK ranges revisited
I have changed all the values in the "Electrolytes and Metabolites" section to the values from Tietz, a reference book widely used in both the US and the UK. Tietz is a US textbook, but in fact was far closer to the so-called "UK" values than the so-called "US" values. All of these "US" values were either unsourced or sourced from 'popular' websites. I hope that that puts this particular discussion to bed. Scolaire 14:37, 14 July 2007 (UTC)
- Unfortunately US laboratories, medical journals and textbooks use US units, so Americans who want to look up a value won't understand them. If you want a peer-reviewed source available online with US units, the Merck Manual has both US units and SI units. Nbauman 03:27, 12 September 2007 (UTC)
- Different discussion, Nbauman. This was about a previous editor saying that urea was 2.5-6.4 mmol/L in the UK but 2.6-6.8 mmol/L in the US, and the same for other analytes, which it turned out was not so much POV as just values plucked from the air (see UK Ranges, above). US units have been included here where appropriate. Scolaire 08:02, 12 September 2007 (UTC)
- Oh, I see now, you have urea in both mmol/L and mg/dL one on top of the other. But if you want a consistent set of both units, you can find it in the Merck Manual. You can also find a consistent set of both units in the New England Journal of Medicine, but I don't know if that's available free to non-subscribers. Nbauman 18:14, 12 September 2007 (UTC)
- I don't know what your problem is with Tietz. It has both sets, it is consistent, and it, rather than the Merck Manual, is the standard reference book in Clinical Biochemistry laboratories in the US and Europe. Scolaire 18:21, 12 September 2007 (UTC)
I agree with scolaire Tietz is by far the most well known clinical chemistry textbook for medical lab science in Ireland and would be considered a very reliable source by medical lab scientists here anyway 109.255.44.47 (talk) 20:55, 24 July 2012 (UTC)
The best current source of reference ranges for the UK is the Pathology Harmony project, which is working to establish consensus reference ranges where possible. It is important to note that for many substances there cannot be one 'correct' reference range, because you get very different answers when you use different analytical methods, for complicated reasons. It is essential to use method specific ranges provided by the lab that did the test. No-one should be routinely referring to ranges from textbooks or the internet. I really feel this article is misleading in not clearly getting that message across. I personally am uncomfortable with this article being here and I think there's little point in it, since most of the ranges aren't of any practical use. Arripay (talk) 22:58, 14 August 2013 (UTC)
- The tables do support different values, even for the same patient type, such as both 6 and 11 ng/ml for the lower limit of progesterone for females in mid-luteal phase. Also, there is a section on variability at Reference_ranges_for_blood_tests#Variability. Still, if we were to go a step further, we could separate values based on the geographic location of the reference group as well, adding another column next to e.g. "female" or "male". Mikael Häggström (talk) 07:01, 15 August 2013 (UTC)
Miller. The problem of getting that in this were to make that decision
the decision is the worst part of getting that many things fine in my personal opinion on my opinion on my opinion Ted does US have the worst thine of course 174.76.177.51 (talk) 15:53, 19 November 2023 (UTC)