User:C.q20n.17/sandbox
 | This is a user sandbox of C.q20n.17. You can use it for testing or practicing edits. This is not the sandbox where you should draft your assigned article for a dashboard.wikiedu.org course. To find the right sandbox for your assignment, visit your Dashboard course page and follow the Sandbox Draft link for your assigned article in the My Articles section. |
Week 7,8,9: Drafting Article with Major Edits[edit]
Major Edits will be bolded and italicized. My edits involve rearranging & adding the order of topics, breaking down the "Discussion section," sentence structure, and location of needed citation:
Original Order of Information:
- 1 Discussion
- 2 Neural control of slow-wave sleep
- 3 Functions of slow-wave sleep
- 3.1 Physical healing and growth
- 3.2 Effects of sleep deprivation
- 4 Problems associated with slow-wave sleep
- 5 Individual differences in slow-wave sleep
- 6 Electroencephalographic characteristics
- 7 See also
- 8 References
Proposed rearrangement:
- 1. Electroencephalographic characteristics
- 2. Functions of slow-wave sleep
- 2.1 Neural control
- 2.2 Physical healing and growth
- 2.3 Learning and Synaptic homeostasis
- 3. Problems associated with slow-wave sleep
- 3.1 Effects of sleep deprivation
- 4. Individual differences
- 5. Drugs
- 6. See also
- 7. References
This is the original article writing with my incorporated edits shown in bold and italic[edit]
Slow-wave sleep (SWS), often referred to as deep sleep, consists of stage three of non-rapid eye movement sleep, according to the Rechtschaffen & Kales (R & K) standard of 1968.[1] There is not a clear distinction between stages three and four. Stage three has 20-50 percent delta activity, whereas stage four has more than 50 percent.[2] As of 2008, the American Academy of Sleep Medicine (AASM) has discontinued the use of stage four,[3][4][5] such that the previous stages three and four now are combined as stage three. An epoch (30 seconds of sleep) which consists of 20% or more slow-wave (delta) sleep is now considered to be stage three.
This period of sleep is called slow-wave sleep because the EEG activity is synchronized, producing slow waves with a frequency of less than 1 Hz and a relatively high amplitude. The first section of the wave signifies a down state, which is an inhibition or hyperpolarizing period phase in which the neurons in the neocortex are silent. This is the period when the neocortical neurons are able to rest. The second section of the wave signifies an "up state," which is an excitation or or depolarizing period phase in which the neurons fire briefly at a high rate. The former state is a hyperpolarizing phase and the latter is a depolarizing phase. The principal characteristics during slow-wave sleep that contrast with REM sleep are moderate muscle tone, slow or absent eye movement, and lack of genital activity.[6]
Slow-wave sleep is considered important to consolidate new memoriesfor memory consolidation.[7] This is sometimes referred to as "sleep-dependent memory processing".[8] Impaired memory consolidation has been effected in individuals with primary insomnia who thus do not perform as well as normal patients in memory tasks following a period of sleep.[9] Furthermore, slow-wave sleep improves declarative memory (which includes semantic and episodic memory). A central model has been hypothesized that the long-term memory storage is facilitated by an interaction between the hippocampal and neocortical networks.[9] In several studies, after the subjects have had training to learn a declarative memory task, the density of human sleep spindles was significantly higher compared to the non-learning control task. This is the result of the spontaneously occurring wave oscillations that account for the intracellular recordings from thalamic and cortical neurons.[10]
[Wikipedia hyperlink for memory consolidation as well as citations have been added for sleep dependent memory processing & insomnia sentence]
Sleep deprivation studies with humans suggest that the primary function of slow-wave sleep may be to allow the brain to recover from its daily activities. Glucose metabolism in the brain increases as a result of tasks that demand mental activity.[11] Another function affected by slow-wave sleep is the secretion of growth hormone, which is always greatest during this stage.[12] It is also thought to be responsible for a decrease in sympathetic and increase in parasympathetic neural activity.[12]
Electroencephalographic characteristics[edit]
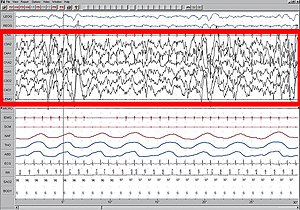
High amplitude EEG is highlighted in red.
Large 75-microvolt (0.5–3 Hz) delta waves predominate the electroencephalogram (EEG). Stage N3 is defined by the presence of 20% delta waves in any given 30-second epoch of the EEG during sleep, by the current 2007 AASM guidelines.[5]
Longer periods of SWS occur in the first part of the night, primarily in the first two sleep cycles (roughly three hours). Children and young adults will have more total SWS in a night than older adults. The elderly may not go into SWS at all during many nights of sleep.
Slow-wave sleep is an active phenomenon probably brought about by the activation of serotonergic neurons of the raphe system.[13]
[Citation added]
The slow wave seen in the cortical EEG is generated through thalamocortical communication through the thalamocortical neurons.[14] In the TC neurons this is generated by the "slow oscillation" and is dependent on membrane potential bistability, a property of these neurons due to an electrophysiological component known as "I t window". "I t window" is due to the overlap underneath activation and inactivation curves if plotted for T-type calcium channels (inward current). If these two curves are multiplied, and another line superimposed on the graph to show a small Ik leak current (outward), then the interplay between these inward (I t window) and outward (small Ik leak), three equilibrium points are seen at −90, −70 and −60 mv, −90 and −60 being stable and −70 unstable. This property allows the generation of slow waves due to an oscillation between two stable points. It is important to note that in in vitro, mGluR must be activated on these neurons to allow a small Ik leak, as seen in in vivo situations.
Discussion[edit]
The highest arousal thresholds (i.e. difficulty of awakening, such as by a sound of a particular volume) are observed in deep sleep. A person will typically feel more groggy when awoken from slow-wave sleep, and indeed, cognitive tests administered after awakening then indicate that mental performance is somewhat impaired for periods of up to 30 minutes, relative to awakenings from other stages. This phenomenon has been called "sleep inertia".
After sleep deprivation there is a sharp rebound of SWS, that is, the following bout of sleep will include more and deeper SWS than normal. The duration of slow-wave sleep is determined by the previous duration of this stage as well as the duration of prior wakefulness.[12]
The major factor determining how much slow-wave sleep is observed in a given sleep period is the duration of preceding wakefulness, likely related to accumulation of sleep-promoting substances in the brain. Some of the factors known to increase slow-wave sleep in the sleep period that follows them include body heating (as by immersion in a hot tub or sauna) and intense prolonged exercise. Studies have shown that slow-wave sleep is enabled when brain temperature surpasses a certain threshold. It is hypothesized that the threshold is regulated by circadian and homeostatic processes.[15] In healthy sleepers, a very low carbohydrate diet over the short-term promotes increases in the percentage of SWS (deep sleep stage four, now often called stage three) and a reduction in the percentage of REM sleep (dreaming sleep) compared to the control with a mixed diet - the sleep changes may be linked to the metabolism of the fat content of the very low carbohydrate diet.[16]
In addition to these factors, the duration of SWS periods can be increased by the ingestion of certain SSRI, and other antidepressants, [citation needed] whereas the effects of THC on SWS remain controversial.[17][18] In instances such as these, total sleep time (TST) is often unaffected due to circadian rhythms, a person's alarm clock, or early morning obligations. This increase of SWS can lead to increased REM latency and a decrease in REM duration. If the total time spent in REM sleep is decreased long enough and repeatedly over a substantial number of nights a "REM rebound" will occur in response to the removal of its inhibitor. An increase in REM sleep is believed to produce symptoms of depression and bipolar disorder in many patients for an amount of time relative to the severity of the previous REM suppression. It is debatable whether this explains the return in symptoms of depression disorder after removal of SSRI medications.
Reduced slow-wave sleep (SWS) may predict high blood pressure in older men.[19]
A study from the Department of Endocrinology at Boston Children's Hospital, an affiliate of Harvard Medical School, indicated that regular deep sleep in children is helpful in triggering the steady release of the hormones that cause puberty.[20] }}
[There should not be a discussion section. The information included in this section are random and unorganized.]
Functions of slow-wave sleep[edit]
Slow-wave sleep is necessary for survival. Some animals, such as dolphins and birds, have the ability to sleep with only one hemisphere of the brain, leaving the other hemisphere awake to carry out normal functions and to remain alert.
Neural control of slow-wave sleep[edit]
Several neurotransmitters are involved in sleep and waking patterns: acetylcholine, norepinephrine, serotonin, histamine, and orexin.[21] Neocortical neurons fire spontaneously during slow-wave sleep, thus they [What is they? the neurotransmitters?] seem to play a role during this period of sleep. Also, these neurons appear to have some sort of internal dialogue, which accounts for the mental activity during this state where there is no information from external signals because of the synaptic inhibition at the thalamic level. The rate of recall of dreams during this state of sleep is relatively high compared to the other levels of the sleep cycle. This indicates that the mental activity is closer to real life events.[10]
[Added "of the sleep cycle" to clarify what "levels" was referring to.]
Physical healing and growth[edit]
Slow-wave sleep is the constructive phase of sleep for recuperation of the mind-body system in which it rebuilds itself after each day. Substances that have been ingested into the body while an organism is awake are synthesized into complex proteins of living tissue. Growth hormones are also secreted to facilitate the healing of muscles as well as repairing damage to any tissues. Lastly, glial cells within the brain are restored with sugars to provide energy for the brain.[22]
Learning and Synaptic Homeostasis[edit]
During wakefulness, learning and memory formation occurs during wakefulness by the process of of long-term potentiation. SWS is associated with the regulation of synapses potentiated during wakefulness. SWS has been studied to be involved in the downscaling of synapses, in which strongly stimulated or potentiated synapses are kept while weakly potentiated synapses either diminish or are removed.[23] This may be helpful for recalibrating synapses for the next potentiation during wakefulness and maintaining synaptic plasticity.
[Added a section about learning and homeostatic synaptic downscaling]
Problems associated with slow-wave sleep[edit]
Bedwetting, night terrors, and sleepwalking are all common behaviors that can occur during stage three of sleep. These occur most frequently amongst children, who then generally outgrow them.[11] Another problem that may arise is sleep-related eating disorder. An individual will sleep-walk leaving his or her bed in the middle of the night seeking out food, and will eat not having any memory of the event in the morning.[11] Over half of individuals with this disorder become overweight.[24] Sleep-related eating disorder can usually be treated with dopaminergic agonists, or topiramate, which is an anti-seizure medication. This nocturnal eating throughout a family suggests that heredity may be a potential cause of this disorder.[11]
Effects of sleep deprivation[edit]
J. A. Horne (1978) reviewed several experiments with humans and concluded that sleep deprivation has no effects on people’s physiological stress response or ability to perform physical exercise. It did, however, have an effect on cognitive functions. Some people reported distorted perceptions or hallucinations and lack of concentration on mental tasks. Thus, the major role of sleep does not appear to be rest for the body, but rest for the brain.
When sleep-deprived humans sleep normally again, the recovery percentage for each stage of sleep is not the same. Only seven percent of stages one and two are regained, but 68 percent of stage-four slow-wave sleep and 53 percent of REM sleep are regained. This suggests that stage-four sleep (known today as the deepest part of stage-three sleep) is more important than the other stages.
During slow-wave sleep, there is a significant decline in cerebral metabolic rate and cerebral blood flow. The activity falls to about 75 percent of the normal wakefulness level. The regions of the brain that are most active when awake have the highest level of delta waves during slow-wave sleep. This indicates rest is geographical. The “shutting down” of the brain accounts for the grogginess and confusion if someone is awakened during deep sleep since it takes the cerebral cortex time to resume its normal functions.[25]
According to J. Siegel (2005), sleep deprivation results in the build-up of free radicals and superoxides in the brain. Free radicals are oxidizing agents that have one unpaired electron, making them highly reactive. These free radicals interact with electrons of biomolecules and damage cells. In slow-wave sleep, the decreased rate of metabolism reduces the creation of oxygen byproducts, thereby allowing the existing radical species to clear. This is a means of preventing damage to the brain.
Individual differences in slow-wave sleep[edit]
Though SWS is fairly consistent within the individual, it can vary across individuals. Age and gender have been noted as two of the biggest factors that affect this period of sleep. Aging is inversely proportional to the amount of SWS beginning by midlife and therefore, SWS declines with age. Sex differences have also been found, such that females tend to have higher levels of SWS compared to males, at least up until menopause. There have also been studies that have shown differences between races. The results showed that there was a lower percentage of SWS in African Americans compared to Caucasians, but since there are many influencing factors (e.g. body mass index sleep-disordered breathing, obesity, diabetes, and hypertension) this potential difference must be investigated further.[26]
Drugs[edit]
The chemical gamma-hydroxybutyric acid (GHB) is known to promote has been studied to increase SWS.[27][28] In the United States, the Food and Drug Administration permits the use of GHB under the trade name Xyrem to reduce cataplexy attacks and excessive daytime sleepiness in patients with narcolepsy.
[Took descriptions from "Discussion section," edited and added a citation.]
See also[edit]
|
References[edit]
Notes
- ^ Rechtschaffen, A; Kales, A (1968). A Manual of Standardized Terminology, Techniques and Scoring System For Sleep Stages of Human Subjects. US Dept of Health, Education, and Welfare; National Institutes of Health.
- ^ Carlson, Neil R. (2012). Physiology of Behavior. Pearson. p. 291. ISBN 0205239390.
- ^ Schulz, Hartmut (2008). "Rethinking sleep analysis. Comment on the AASM Manual for the Scoring of Sleep and Associated Events". J Clin Sleep Med. 4 (2). American Academy of Sleep Medicine: 99–103. PMC 2335403. PMID 18468306.
Although the sequence of non-REM (NREM) sleep stages one to four (R&K classification) or N1 to N3 (AASM classification) fulfills the criteria...
- ^ "Glossary. A resource from the Division of Sleep Medicine at Harvard Medical School, Produced in partnership with WGBH Educational Foundation". Harvard University. 2008. Retrieved 2009-03-11.
The 1968 categorization of the combined Sleep Stages 3 - 4 was reclassified in 2007 as Stage N3.
- ^ a b Iber, C; Ancoli-Israel, S; Chesson, A; Quan, SF. for the American Academy of Sleep Medicine. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. Westchester: American Academy of Sleep Medicine; 2007.
- ^ Carlson, Neil R. (2012). Physiology of Behavior. Pearson. p. 291,293. ISBN 0205239390.
- ^ https://www.nytimes.com/2013/01/28/health/brain-aging-linked-to-sleep-related-memory-decline.html
- ^ Walker, Matthew P. (1 January 2008). "Sleep-dependent memory processing". Harvard Review of Psychiatry. 16 (5): 287–298. doi:10.1080/10673220802432517. ISSN 1465-7309.
- ^ a b http://walkerlab.berkeley.edu/reprints/Walker_JCSM_2009.pdf
- ^ a b http://www.architalbiol.org/aib/article/viewFile/411/370
- ^ a b c d Carlson, Neil R. (2012). Physiology of Behavior. Pearson. pp. 297–298. ISBN 0205239390.
- ^ a b c Slow-Wave Sleep: Beyond Insomnia. Wolters Kluwer Pharma Solutions. ISBN 978-0-9561387-1-2.
- ^ Jones, BE (1 May 2003). "Arousal systems". Frontiers in bioscience : a journal and virtual library. 8: s438-51. ISSN 1093-9946. PMID 12700104.
- ^ Williams SR, Tóth TI, Turner JP, Hughes SW, Crunelli W (1997) The window component of the low threshold Ca2+ current produces input signal amplification and bistability in cat and rat thalamocortical neurones. J Physiol 505:689–705.
- ^ McGinty, Dennis; Ronald Szymusiak (1990). "Keeping cool: a hypothesis about the mechanisms and functions of slow-wave sleep". Science Direct. Trends in Neuroscience. 13 (12): 480–487. doi:10.1016/0166-2236(90)90081-k.
- ^ Afaghi A, O'Connor H, Chow CM (August 2008). "Acute effects of the very low carbohydrate diet on sleep indices". Nutr Neurosci. 11 (4): 146–54. doi:10.1179/147683008X301540. PMID 18681982.
- ^ Schierenbeck, T.; Riemann, D.; Berger, M.; Hornyak, M. (Oct 2008). "Effect of illicit recreational drugs upon sleep: cocaine, ecstasy and marijuana". Sleep Med Rev. 12 (5): 381–389. doi:10.1016/j.smrv.2007.12.004. PMID 18313952.
- ^ Gates, P.J.; Albertella, L.; Copeland, J. (Feb 2014). "The effects of cannabinoid administration on sleep: a systematic review of human studies". Sleep Med Rev. 18: 477–487. doi:10.1016/j.smrv.2014.02.005. PMID 24726015.
- ^ http://www.brighamandwomens.org/about_bwh/publicaffairs/news/pressreleases/PressRelease.aspx?sub=0&PageID=942
- ^ http://www.massgeneral.org/about/pressrelease.aspx?id=1502
- ^ Carlson, Neil R. (2012). Physiology of Behavior. Pearson. p. 305-307. ISBN 0205239390.
- ^ http://www.hgi.org.uk/archive/sleepanddream1.htm#.U2kpm8fhjys
- ^ Tononi, Giulio; Cirelli, Chiara (February 2006). "Sleep function and synaptic homeostasis". Sleep Medicine Reviews. 10 (1): 49–62. doi:10.1016/j.smrv.2005.05.002. PMID 16376591.
- ^ Carlson, Neil R. (2012). Physiology of Behavior. Pearson. p. 298. ISBN 0205239390.
- ^ Carlson, Neil R. (2012). Physiology of Behavior. Pearson. p. 299-300. ISBN 0205239390.
- ^ http://onlinelibrary.wiley.com/enhanced/doi/10.1111/j.1365-2869.2011.00959.x/
- ^ Roehrs, Timothy; Roth, Thomas (December 2010). "Drug-Related Sleep Stage Changes: Functional Significance and Clinical Relevance". Sleep Medicine Clinics. 5 (4): 559–570. doi:10.1016/j.jsmc.2010.08.002. PMID PMC3041980.
{{cite journal}}: Check|pmid=value (help) - ^ http://www.theodora.com/drugs/eu/xyrem.html
Further reading
- M. Massimini, G. Tononi, et al., "Breakdown of Cortical Effective Connectivity During Sleep," Science, vol. 309, 2005, pp. 2228–32.
- P. Cicogna, V. Natale, M. Occhionero, and M. Bosinelli, "Slow Wave and REM Sleep Mentation," Sleep Research Online, vol. 3, no. 2, 2000, pp. 67–72.
- D. Foulkes et al., "Ego Functions and Dreaming During Sleep Onset," in Charles Tart, ed., Altered States of Consciousness, p. 75.
- Rock, Andrea (2004). The Mind at Night.
- Warren, Jeff (2007). "The Slow Wave". The Head Trip: Adventures on the Wheel of Consciousness. ISBN 978-0-679-31408-0.
Category:Sleep physiology Category:Electroencephalography Category:Biology of bipolar disorder Category:Articles containing video clips
Week 6: Expanding on Article Edits[edit]
For the discussion section, mentioned in the Week 5 notes, there needs to be more source(s) to support the arousal threshold of "deep sleep." This phrase seems a little vague on whether deep sleep is SWS NREM or REM sleep.
Vander's Human Physiology textbook talks about REM sleep EEG patterns showing intense activity/arousal similar to alert wakefulness. It also discusses O2 consumed by the brain during REM, which supports information about arousal-like activities. However, I'm not sure if this part of the discussion will be helpful for relevance of SWS.
I think that the Discussion section should be rearranged to be at the end of the article instead of the top. It seems to fit there better because discussions. Thoughts?
I will continue to add my expanded edits in the sandbox.[edit]
Week 5: Drafting an Existing Article[edit]
These are some edits that I would like to make in the "Slow-Wave Sleep" article -- I will look for more[edit]
In the second paragraph of the leading section, the explanation about the down state and up state needs to be cleaned up.
- I plan to italicize the words "down" and "up" to make the sentences a little more clear to read
- I will delete the sentence about the former and latter state" because it is redundant.
The wording of the first sentence in the second paragraph of the leading section looks similar to that of the New York Times article that is cited.
- Question Should I rewrite, "Slow-wave is considered to be important for memory consolidation" and link to the "Memory Consolidation" wiki page instead?
The sentence in the third paragraph of the leading section is very similar to the cited reference:
- sentence: "Impaired memory consolidation has been effected in individuals with primary insomnia who thus do not perform as well as normal patients in memory tasks following a period of sleep"
- Walker (2009): " Indeed, impaired memory consolidation has been demonstrated in patients with primary insomnia; such patients do not perform as well as healthy control subjects in tests of memory following a period of sleep"
* **might need to change this: either add a citation about what primary insomnia is or a wikipedia article on insomnia
- --> I was reading through the article by Ceklic and Bastien (2015) in the Effects of Sleep Deprivation section to see if anything could be used
- This article talks about information processing during NREM sleep and insomnia patients
- The hypothesis was that when the sleep quality is the same for good sleepers and insomnia sufferers, then there would be no significant difference in information processing
- The authors mention that the study overall did not show a significance of overall sleep quality between subjects who were good sleepers and insomnia sufferers
- They also mention that their results were indicating some alteration in the inhibition of information processing among the insomnia sufferers, but the authors suggested that the study by Terzano et al. (1990) needs to be reproduced
- the finding is different from the hypothesis
The first paragraph in the Discussion section will need a citation to support the statements about the highest arousal thresholds and the feeling of grogginess
- I will look for information in the Vander's Human Physiology textbook to see if it can support this
Functions of Slow-Wave Sleep section:
- I might incorporate the article by Tononi and Cirelli (2005), which talks about the hypothesis of slow wave activity and synaptic downscaling after learning or potentiation during wakefulness.
- This article mentions that Slow wave sleep is involved in keeping the highly long-term potentiated synapses while downscaling or removing the weakly potentiated synapses. This might be helpful with the current statements in the leading section about memory consolidation and up and down states.
- This article also mentions that the downscaling of synaptic strength to a baseline is helpful in recalibrating the synapses and thus start the cycle of potentiation again during wakefulness.
- On page 55 of the article, the important functions of sleep with synaptic pruning is energy and space -- I will at the cited references to make sure the statements are interpreted correctly
C.q20n.17 (talk) 16:49, 22 February 2017 (UTC)
Week 4: Choose your topic / Find your sources[edit]
The article that I would like to work on is called Slow-Wave Sleep. One thing I can look forward to editing is elaborating on/modifying explanations.
Some sources that I will look through and might use are textbook, Vander's Human Physiology: The Mechanisms of Body Function, a theoretical review article, "Sleep Function and Synaptic Homeostasis" by Tononi and Cirelli (2006), and "Information processing during NREM sleep and sleep quality in insomnia" by Ceklic and Bastian (2015).
I will continue to look for more sources to support the statements with relevant sources.
C.q20n.17 (talk) 05:25, 15 February 2017 (UTC)
Week 2: Evaluating Articles and Sources Assignment: Reviewing Physiology article[edit]
1. Is each fact referenced with an appropriate, reliable reference?
The first reference comes from an online etymology website called etymonline.com, which sources from many other sources for terminology. It would be beneficial to look through the list of sources on this website that the website uses to describe “physiology” in order to make sure that the Wikipedia article is not closely paraphrasing these primary sources.
Also, reference #20 about the Cori cycle comes from TheFreeDictionary.com, which has a page of different sources with differently phrased definitions about the Cori cycle. The reference for the article might need a more specific to one of the listed, reliable sources to support the information.
2. Is everything in the article relevant to the article topic? Is there anything that distracted you?
The information currently in the physiology article are relevant to understanding the history of physiology from theory to practice, but the article seems to focus more on history than the general scientific topics taught in physiology classes today.
The history section contains a huge paragraph combining the theories of Hippocrates, Galenus, Aristotle, and Galen, which makes it difficult to read and is different from the shorter sections following this paragraph. I would break up the one paragraph into smaller parts so that readers know that the consecutive thinkers added onto the theory of physiology.
There are variations between adding the reference citation number at the beginning or at the end of facts. It would good formatting-wise to keep the reference positions consistent.
Furthermore, the list of female physiologists’ contributions seemed very compact with detail on their works and no spaces in between each bullet point.
3. Is the article neutral? Are there any claims, or frames, that appear heavily biased toward a particular position?
The sources are primarily from textbooks, other encyclopedias, and publications. However, as mentioned in the response for question 1, sources such as the etymology section are a culmination of other references. It would be good to check earlier references to make sure that close paraphrasing is avoided as much as possible. The article focuses a lot on women’s contribution in the studying of physiology rather than a list of many of the documented physiologists, both female and male, that contributed to today’s research and teachings about physiology.
4. Where does the information come from? Are these neutral sources? If biased, is that bias noted?
Most of the cited information comes from other Wikipedia articles and online encyclopedias (ex: Encyclopedia Britannica), textbooks, publications, and websites with their own listed references. The sources are mostly neutral sources.
5. Are there viewpoints that are overrepresented, or underrepresented?
The section transition from “History” to “Women in Physiology” is a little abrupt as to how women became prominent in the studying of physiology. It would be nice to see a list of both female and male physiologists organized by common subdisclipines to provide a more inclusive format to the studies and contributions that were made.
6. Check a few citations. Do the links work? Is there any close paraphrasing or plagiarism in the article?
Reference #13 “Milestones in Physiology (1822-2013)” needs to be updated because the link does not show the pdf on Physiologyinfo.org with the cited information.
Some of the sentences listing contributions by female physiologists like Barbara McClintock, are paraphrased to what is said in the Wikipedia articles that were linked. One thing that would help avoid this is to create a schematic with a timeline of prominent physiologists.
7. Is any information out of date? Is anything missing that could be added?
Under the “Women in Physiology” section, there still needs to be a citation added to the second and third sentences. In addition, the following paragraph starting with, “Soon thereafter, in 1913…” needs be cited.
For missing data, I think it would help if in the “Women in physiology” section, a sentence were added after listing the six women admitted in The Physiological Society generally about the topics that these female physiologists studied. This would help to introduce the bulleted list of studies by these physiologists.
8. How does the Wikipedia article compare to the ways we've discussed this topic in class? Does it align? What information might be incorrect or missing?
There are a few names of physiologists that we’ve briefly discussed in class such as Claude Bernard, as well as the origin of the word physiology. Yet, the “Human Physiology” section of the article has few references to support the information provided in the two paragraphs, so there needs to more textbook and academic press references added.
Also, there needs to be an elaboration of information about the studied systems in the human body (ex: digestive, urinary, reproductive, circulatory, etc.).
