Mitochondrial myopathy
| Mitochondrial myopathy | |
|---|---|
| Other names | Mitochondrial muscle disease; muscle mitochondrinopathy; muscle mitochondrial dysfunction |
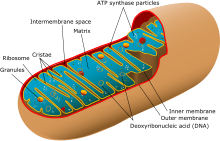 | |
| Simplified structure of a typical mitochondrion | |
| Specialty | Neuromuscular medicine |
Mitochondrial myopathies are types of myopathies associated with mitochondrial disease.[1] Adenosine triphosphate (ATP), the chemical used to provide energy for the cell, cannot be produced sufficiently by oxidative phosphorylation when the mitochondrion is either damaged or missing necessary enzymes or transport proteins. With ATP production deficient in mitochondria, there is an over-reliance on anaerobic glycolysis which leads to lactic acidosis either at rest or exercise-induced.[2]
Primary mitochondrial myopathies are inherited, while secondary mitochondrial myopathies may be inherited (e.g. Duchenne's muscular dystrophy)[3] or environmental (e.g. alcoholic myopathy[4][5]). When it is an inherited primary disease, it is one of the metabolic myopathies.[6][4]
On biopsy, the muscle tissue of patients with these diseases usually demonstrate "ragged red" muscle fibers on Gomori trichrome staining. The ragged-red appearance is due to a buildup of abnormal mitochondria underneath the plasma membrane.[7] These ragged-red fibres may contain normal or abnormally increased accumulations of glycogen and neutral lipids, with histochemical staining showing abnormal respiratory chain involvement, such as decreased succinate dehydrogenase or cytochrome c oxidase.[8] Inheritance was believed to be maternal (non-Mendelian extranuclear). It is now known that certain nuclear DNA deletions can also cause mitochondrial myopathy such as the OPA1 gene deletion.[6]
Signs and symptoms[edit]
Proximal muscle weakness, exercise intolerance, lactic acidosis, high serum lactate/pyruvate ratio, normal to elevated serum CK, dyspnea, exaggerated cardiorespiratory response to exercise are common symptoms. It may be isolated to the muscle (pure myopathy) or may be systemic including not only myopathy, but also eye abnormalities, peripheral neuropathy, and neurological abnormalities. Muscle biopsy typically shows ragged-red fibres, histochemical staining shows abnormality of respiratory chain or decreased cytochrome c oxidase (COX).[9][10]
The five most common are MELAS, MERF, KSS, CPEO, and MNGIE which are listed below:[9]
- Mitochondrial encephalomyopathy, lactic acidosis, and stroke-like syndrome (MELAS)
- Varying degrees of cognitive impairment and dementia
- Lactic acidosis
- Strokes
- Transient ischemic attacks
- Hearing loss
- Weight loss
- Myoclonic epilepsy and ragged-red fibers (MERRF)
- Progressive myoclonic epilepsy
- Clumps of diseased mitochondria accumulate in muscle fibers and appear as "ragged-red fibers" when muscle is stained with modified Gömöri trichrome stain
- Short stature
- Kearns–Sayre syndrome (KSS)
- External ophthalmoplegia
- Cardiac conduction defects
- Sensorineural hearing loss
- Chronic progressive external ophthalmoplegia (CPEO)
- Progressive ophthalmoparesis
- Symptomatic overlap with other mitochondrial myopathies
- Mitochondrial neurogastrointestinal encephalopathy (MNGIE)
- Muscle weakness and atrophy, more prominent distally
- Hyporeflexic or areflexic
- Ptosis and ophthalmoparesis common
- Gastrointestinal dysmotility (such as bloating, stomach cramps, diarrhea)
Cause[edit]
Mitochondrial myopathy literally means mitochondrial muscle disease, muscle disease caused by mitochondrial dysfunction. The mitochondrion is the primary producer of energy in nearly all cells throughout the body. The exception is mature erythrocytes (red blood cells), so that they do not use up the oxygen that they carry. In the eye, the lens and outer segment of the retina contain almost no mitochondria. Muscle cells have many mitochondria, particularly type I muscle fibres, and if the mitochondria have problems by which they do not produce enough energy for the cell to function, problems occur.[11]
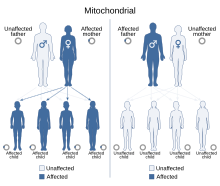
The cause may be genetic, with many having mitochondrial inheritance (involving the mitochondrial DNA which is only passed on from the mother), although nuclear DNA mutations with Mendelian inheritance that are either autosomal dominant, recessive, or X-linked recessive also exist. A nuclear DNA example is a mutation within the POLG (polymerase gamma) gene, which causes mitochondrial DNA (mtDNA) to become damaged and lose function.
Disease list[edit]
| Name
(alternate names) |
Gene(s) | Inheritance pattern
(MT, AR, AD, X-Linked) |
OMIM #
(GD: gene description, PS: phenotypic series) |
|---|---|---|---|
| Mitochondrial encephalomyopathy, lactic acidosis, and stroke-like syndrome (MELAS)
(Juvenile myopathy, encephalopathy, lactic acidosis and stroke) |
MT-TL1, MT-TQ, MT-TH, MT-TK, MT-TC, MT-TS1, MT-ND1, MT-ND5, MT-ND6, MT-TS2 | MT | 540000[12] |
| Myoclonic epilepsy and ragged-red fibers (MERRF) | MT-TK, MT-TL1, MT-TH, MT-TS1, MT-TS2, MT-TF | MT | 545000[13] |
| Kearns–Sayre syndrome (KSS)
(Ophthalmoplegia, pigmentary degeneration of retina, and cardiomyopathy; oculocraniosomatic syndrome; ophthalmoplegia-plus syndrome; mitochondrial cytopathy, ophthalmoplegia, progressive external, with ragged-red fibers; chronic progressive external ophthalmoplegia with myopathy; CPEO with myopathy; CPEO with ragged-red fibers) |
MT-TL1 | MT | 530000[14] |
| Chronic progressive external ophthalmoplegia (CPEO)
(Progressive external ophthalmoplegia with mitochondrial DNA deletions, autosomal recessive/dominant) |
POLG, SLC25A4, RNASEH1, TWNK, TK2, POLG2, DGUOK, TOP3A, RRM2B | AR/AD | PS157640[15] |
| Mitochondrial DNA depletion syndrome (MNGIE type)
(Mitochondrial neurogastrointestinal encephalopathy (MNGIE); myoneurogastrointestinal encephalopathy syndrome; polyneuropathy, ophthalmoplegia, leukoencephalopathy, and intestinal pseudoobstruction; POLIP syndrome) |
TYMP, RRM2B, POLG, LIG3 | AR | 603041;
612075; 613662; 619780[16] |
| Mitochondrial DNA depletion syndrome
(Alpers type, cardiomyopathic type, encephalomyopathic type, hepatocerebral type, and myopathic type) |
MGME1, SLC25A10, TK2, POLG, SLC25A21, SUCLA2, TWNK, TFAM, AGK, MRM2, SLC25A4, OPA1, SUCLG1 | AR/AD | PS603041[16] |
| Mitochondrial myopathy, infantile, transient (MMIT)
(Mitochondrial myopathy, infantile, transient, due to respiratory chain deficiency; COX deficiency myopathy, infantile, transient; respiratory chain deficiency, infantile, transient) |
MT-TE | MT | 500009[17] |
| Mitochondrial myopathy, lethal, infantile (LIMM)
(Lethal infantile mitochondrial myopathy) |
MT-TT | MT | 551000[18] |
| Hereditary myopathy with lactic acidosis (HML)
(Myopathy with exercise intolerance, Swedish type; myopathy with deficiency of succinate dehydrogenase and aconitase; myoglobinuria due to abnormal glycolysis; Larsson–Linderholm syndrome; Linderholm myopathy) |
ISCU | AR/AD[19] | 255125[20] |
| Mitochondrial myopathy with diabetes
(Mitochondrial myopathy, lipid type) |
MT-TE | MT | 500002[21] |
| Maternally inherited diabetes and deafness (MIDD)
(Diabetes and deafness (DAD); Ballinger–Wallace syndrome; Noninsulin-dependent diabetes mellitus with deafness, maternally inherited) |
MT-TL1, MT-TE, MT-TK | MT | 520000[22] |
| Myopathy, mitochondrial progressive, with congenital cataract and developmental delay (MPMCD)
(Myopathy with cataract and combined respiratory chain deficiency; mitochondrial complex deficiency, combined) |
GFER | AR | 613076[23] |
| Myopathy, lactic acidosis, and sideroblastic anemia (MLASA)
(Mitochondrial myopathy and sideroblastic anemia) |
PUS1, YARS2, MT-ATP6 | AR/MT | 600462
613561[24] GD: 516060[25] |
| Myopathy, isolated mitochondrial, autosomal dominant (IMMD) | CHCHD10 | AD | 616209[26] |
| Myopathy, mitochondrial, and ataxia (MMYAT) | MSTO1 | AR/AD | 617675[27] |
| Mitochondrial myopathy, episodic, with or without optic atrophy and reversible leukoencephalopathy (MEOAL) | FDX2 | AR | 251900[28] |
| Mitochondrial myopathy with lactic acidosis (MMLA) | PNPLA8 | AR | 251950[29] |
| Mitochondrial myopathy with a defect in mitochondrial-protein transport | Unknown | AR | 251945[30] |
| Myotonic dystrophy-like myopathy;
Mitochondrial myopathy |
MT-TA | MT | GD: 590000[31] |
| Mitochondrial myopathy, isolated | MT-TD | MT | GD: 590015[32] |
| Myopathy, mitochondrial | MT-TW | MT | GD: 590095[33] |
| Coenzyme Q10 deficiency, primary (COQ10D)
(CoQ10 deficiency, primary; ubiquinone deficiency; Coenzyme Q deficiency; CoQ deficiency) |
COQ2, PDSS1, PDSS2, ADCK3, COQ9, COQ4, COQ7, COQ5 | AR | PS607426[34] |
| Mitochondrial complex I deficiency, nuclear type (MC1DN)
(NADH:Q(1) oxidoreductase deficiency; NADH-coenzyme Q reductase deficiency; mitochondrial NADH dehydrogenase component of complex I, deficiency of) |
NDUFS2, NDUFB3, NDUFS1, NDUFA10, NDUFAF3, TIMMDC1, ACAD9, NDUFS6, NDUFS4, NDUFAF2, NDUFA2, NDUFAF4, DNAJC30, NDUFAF6, NDUFB9, NDUFA8, NDUFB8, NDUFS3, NDUFV1, NDUFS8, NDUFC2, TMEM126B, FOXRED1, NDUFA9, NDUFA12, NUBPL, NDUFAF1, MTFMT, NDUFB10, NDUFAF8, NDUFV2, NDUFS7, NDUFA11, NDUFB7, NDUFA13, NDUFAF5, NDUFA6, NDUFB11, NDUFA1 | AR/XL/XLR | PS252010[35] |
| Mitochondrial complex II deficiency, nuclear type (MC2DN)
(Succinate CoQ reductase deficiency; succinate dehydrogenase deficiency) |
SDHA, SDHAF1, SDHD, SDHB | AR | PS252011[36] |
| cytochrome b of complex III (MTCYB);
Exercise intolerance; multisystem disorder; cardiomyopathy, infantile histiocytoid; exercise intolerance, cardiomyopathy, and septooptic dysplasia; parkinsonism/MELAS overlap syndrome |
MT-CYB | MT | GD: 516020[37] |
| Mitochondrial complex III deficiency, nuclear type (MC3DN) | BCS1L, TTC19, UQCRQ, UQCRC2, CYC1, UQCC2, LYRM7, UQCC3, UQCRFS1 | AR | PS124000[38] |
| Mitochondrial complex IV deficiency, nuclear type (MC4DN)
(mitochondrial complex IV deficiency; cytochrome c oxidase deficiency; COX deficiency) |
SURF1, SCO2, COX10, SCO1, LRPPRC, COX15, COX6B1, TACO1, COX14, COX20, PET100, COA6, COA3, COX8A, COX4I1, APOPT1, COX6A2, PET117, COX5A, COXFA4, COX16, COX11 | AR | PS220110[39] |
| Mitochondrial complex V (ATP synthase) deficiency, nuclear type (MC5DN) | ATPAF2, TMEM70, ATP5E, ATP5F1A, ATP5F1D, ATP5MD, ATP5PO | AR/AD | PS604273[40] |
| Muscular dystrophy, limb-girdle, type 1H
(As of 2017 was excluded from LGMD for showing histochemical evidence of being a mitochondrial myopathy, but not yet assigned new nomenclature)[41][42] |
Chromosome 3 (3p23-p25), unknown gene | AD | 613530[43] |
Diagnosis[edit]

Muscle biopsy: usually ragged red fibres in Gömöri trichrome stain, normal or excessive glycogen or lipid accumulation within these ragged red fibres, histochemical staining showing impairment of respiratory chain such as COX-negative fibres.[6][8] Some mitochondrial myopathies are limited to disease expression only in skeletal muscle, with fibroblasts (from skin biopsy) appearing normal.[44][19]
Blood tests: lactate/pyruvate ratio may be elevated or normal, creatine kinase (CK) may be elevated or normal.[6][2] Electrolyte panel, anion gap, glucose, vitamin D, TSH, anti-HMGCR and AChR autoantibodies to rule-out pseudometabolic myopathies.[6][2]
Exercise stress test: exaggerated cardiorespiratory response to exercise (inappropriate rapid heart rate response to exercise with breathlessness [tachycardia and dyspnea]).[10]
DNA tests: whole exome sequencing (WES) neuromuscular panels (that only test exons), or whole genome sequencing (WGS) for more complex cases (that test exons, introns, and mitochondrial DNA). Introns were initially thought to be "junk DNA," however, some introns regulate the expression of exons.[45][46] For example, in the mitochondrial myopathy of hereditary myopathy with lactic acidosis (HML), the most common pathogenic mutation is the intronic IVS5+382 G>C (rs767000507).[19]
There are two groups of DNA that affect the mitochondria: mitochondrial genome (mtDNA) and nuclear DNA.[6] For mitochondrial myopathies that involve a single mtDNA deletion, it would only be found on muscle-derived mtDNA, making a biopsy of affected muscle necessary for DNA analysis rather than saliva or blood.[6][8] Even among siblings with the same inherited mutation, different muscle groups were affected, with unaffected tissues having near normal levels of mtDNA.[47][48]
EMG: may be normal, myopathic, or rarely neurogenic.[6]
The symptoms of exercise intolerance, abnormal muscle fatigue, myalgia (muscle pain), arrhythmia, possible fixed proximal muscle weakness, lipid deposits, possible episodes of rhabdomyolysis, with symptoms becoming evident or worsening while fasting, during a fever, during low-intensity aerobic activity or after prolonged activity–all these overlap with the symptoms of another metabolic myopathy, that of fatty acid metabolism disorders.[6]
DNA testing is helpful for determining between the similar presenting, but different in bioenergetic system origin, metabolic myopathies. When DNA testing is inconclusive, a muscle biopsy is necessary.[2][6][8]
Differential diagnoses[edit]
Diseases that mimic the symptoms of mitochondrial myopathy include electrolyte imbalance, myasthenia gravis, thyroid abnormalities, vitamin D deficiency, immune-mediated necrotizing myopathy, diabetes-related pseudohypoxia, and fatty acid metabolism disorders.[6][2] Hypoxia due to ischemia (insufficient blood flow) also impairs oxidative phosphorylation, which can be seen in intermittent claudication, chronic venous insufficiency, and popliteal artery entrapment syndrome. If symptoms of muscle fatigue improve after approximately 10 minutes of low-moderate intensity aerobic exercise, or after approximately 10 minutes of rest following aerobic exercise, this would be indicative of the second wind phenomenon seen in select muscle glycogenoses.[2]
Ragged red fibres (a mitochondrial abnormality) can be found in a number of myopathies other than the inherited primary mitochondrial myopathies.[49] These include axonal Charcot–Marie–Tooth disease types 2CC & 2EE, congenital myasthenic syndrome types 12 & 14, congenital myopathy types 10B & 22A, and MYH7-related myopathies such as Laing distal myopathy and myosin storage myopathy.[49]
Secondary mitochondrial myopathy can be caused by natural aging,[50][51] inflammatory myopathies,[50] and chronic alcohol use disorder.[4][5] It can also be due to certain drugs such statins, bupivacaine, antiepileptic drugs (phenytoin, valproic acid, and lamotrigine), and nucleoside reverse transcriptase inhibitors (antiviral drugs) such as zidovudine and clevudine.[52]
Some metabolic myopathies affect multiple bioenergetic pathways, for instance multiple acyl-CoA dehydrogenase deficiency (MADD), formerly known as glutaric acidemia type II (GA-II). The ETF genes involved in MADD impairs beta oxidation (fatty acid metabolism), impairs amino acid catabolism (protein metabolism), and simultaneously impairs the respiratory chain by not transferring electrons from reduced FAD+/FADH2. The impaired protein metabolism leads to a buildup of glutaric acid and other acids. Fatty acid metabolism is further impaired as carnitine is used to detoxify the buildup of glutaric acid, causing secondary carnitine deficiency.[53][54] Although MADD affects multiple bioenergetic pathways, it is classified as a fatty acid metabolism disorder as that is the bioenergetic pathway that is affected the most by the deficiency. However, it is important to note as a differential diagnosis as not only do the symptoms overlap with mitochondrial myopathies, but also muscle biopsies of some individuals with MADD show COX-negative fibres, respiratory chain impairment, and deficiency of coenzyme Q10.[55][56] Some forms of MADD respond well to riboflavin, known as riboflavin-responsive MADD (RR-MADD).[6]
Riboflavin-responsive exercise intolerance (RREI), a fatty acid metabolism disorder involving the SLC25A32 gene, has symptoms similar to MADD, with muscle biopsy showing ragged red fibres and lipid deposits (mainly in type I fibres), small type II fibres, and impaired FAD-dependent mitochondrial respiratory chain.[57]
Pompe disease (glycogen storage disease type II), another type of metabolic myopathy, has secondary mitochondrial dysfunction present in both the earlier onset forms (infantile and juvenile) and the late-onset form in adults.[58]
Myopathies involving the DMD gene, such as Duchenne and Becker muscular dystrophy, have secondary mitochondrial dysfunction impairing oxidative phosphorylation.[3][59] The mechanisms leading to this mitochondrial dysfunction are many and it has yet to be elucidated which mitochondrial changes are directly due to the disease and which are compensatory.[3] Three unrelated young boys, with a mutation in the DMD gene, exhibited a pseudometabolic presentation with symptoms of exercise intolerance manifesting as exercise-induced myalgia, muscle stiffness, myoglobinuria and rhabdomyolysis.[60]
A few Limb–girdle muscular dystrophies are known to have secondary mitochondrial dysfunction, including: LGMDR1 calpain3-related (formerly LGMD 2A), LGMDR2 dysferlin-related (LGMD 2B), LGMDR3 α-sarcoglycan-related (LGMD 2D), LGMDR5 γ-sarcoglycan-related (LGMD 2C), and LGMDR6 δ-sarcoglycan-related (LGMD 2F).[59][61] As well as Myofibrillar myopathy 8 (MFM8) PYROXD1-related, which has an adult-onset, slowly progressive, Limb–girdle phenotype.[59][62]
Treatment[edit]
Although no cure currently exists, there is hope in treatment for this class of hereditary diseases as trials continue.
Aerobic training may improve oxidative capacity by the skeletal muscles becoming aerobically conditioned. Deoxynucleoside monophosphates and deoxynucleotide taken orally, may help in TK2 deficiency (Mitochondrial DNA depletion syndrome 2 myopathic type).[6]
Avoiding physically stressful situations that deplete glycogen reserves, such as fasting and endurance exercise (which rely predominantly on oxidative phosphorylation), may help. A high-carb/low-fat/low-protein diet may help.[6]
See also[edit]
References[edit]
- ^ "Mitochondrial Myopathy Information Page | National Institute of Neurological Disorders and Stroke". www.ninds.nih.gov. Retrieved 2017-02-28.
- ^ a b c d e f Bhai S (September 2021). "Neuromuscular Notes: Diagnosing Metabolic Myopathies". Practical Neurology.
- ^ a b c Heydemann A (June 2018). "Skeletal Muscle Metabolism in Duchenne and Becker Muscular Dystrophy-Implications for Therapies". Nutrients. 10 (6): 796. doi:10.3390/nu10060796. PMC 6024668. PMID 29925809.
- ^ a b c Simon L, Jolley SE, Molina PE (2017). "Alcoholic Myopathy: Pathophysiologic Mechanisms and Clinical Implications". Alcohol Research. 38 (2): 207–217. PMC 5513686. PMID 28988574.
- ^ a b Song BJ, Akbar M, Abdelmegeed MA, Byun K, Lee B, Yoon SK, Hardwick JP (2014-01-01). "Mitochondrial dysfunction and tissue injury by alcohol, high fat, nonalcoholic substances and pathological conditions through post-translational protein modifications". Redox Biology. 3: 109–123. doi:10.1016/j.redox.2014.10.004. PMC 4297931. PMID 25465468. S2CID 17113550.
- ^ a b c d e f g h i j k l m n Urtizberea JA, Severa G, Malfatti E (April 2023). "Metabolic Myopathies in the Era of Next-Generation Sequencing". Genes. 14 (5): 954. doi:10.3390/genes14050954. PMC 10217901. PMID 37239314.
- ^ "Ragged-red muscle fibers - MedGen - NCBI". www.ncbi.nlm.nih.gov. Retrieved 2024-01-05.
- ^ a b c d Sarnat, Harvey B.; Marín-García, José (May 2005). "Pathology of Mitochondrial Encephalomyopathies". Canadian Journal of Neurological Sciences. 32 (2): 152–166. doi:10.1017/S0317167100003929. ISSN 0317-1671. PMID 16018150. S2CID 1922603.
- ^ a b Tobon A (December 2013). "Metabolic myopathies". Continuum. 19 (6 Muscle Disease): 1571–1597. doi:10.1212/01.CON.0000440660.41675.06. PMC 10563931. PMID 24305448. S2CID 11050341.
- ^ a b Noury JB, Zagnoli F, Petit F, Marcorelles P, Rannou F (May 2020). "Exercise efficiency impairment in metabolic myopathies". Scientific Reports. 10 (1): 8765. Bibcode:2020NatSR..10.8765N. doi:10.1038/s41598-020-65770-y. PMC 7260200. PMID 32472082.
- ^ "Nutrient Metabolism, Human | Learn Science at Scitable". www.nature.com. Retrieved 2024-04-05.
- ^ "#540000 - MITOCHONDRIAL MYOPATHY, ENCEPHALOPATHY, LACTIC ACIDOSIS, AND STROKE-LIKE EPISODES; MELAS". www.omim.org. Retrieved 2023-11-24.
- ^ "#545000 - MYOCLONIC EPILEPSY ASSOCIATED WITH RAGGED-RED FIBERS; MERRF". www.omim.org. Retrieved 2023-11-24.
- ^ "#530000 - KEARNS-SAYRE SYNDROME; KSS". www.omim.org. Retrieved 2023-11-24.
- ^ "Phenotypic Series - PS157640 - CPEO - OMIM". www.omim.org. Retrieved 2023-11-24.
- ^ a b "Phenotypic Series - PS603041 - Mitochondrial DNA depletion syndrome - OMIM". www.omim.org. Retrieved 2023-11-24.
- ^ "#500009 - MITOCHONDRIAL MYOPATHY, INFANTILE, TRANSIENT; MMIT". www.omim.org. Retrieved 2023-11-24.
- ^ "#551000 - MITOCHONDRIAL MYOPATHY, LETHAL, INFANTILE; LIMM". www.omim.org. Retrieved 2023-11-30.
- ^ a b c Legati, Andrea; Reyes, Aurelio; Ceccatelli Berti, Camilla; Stehling, Oliver; Marchet, Silvia; Lamperti, Costanza; Ferrari, Alberto; Robinson, Alan J.; Mühlenhoff, Ulrich; Lill, Roland; Zeviani, Massimo; Goffrini, Paola; Ghezzi, Daniele (December 2017). "A novel de novo dominant mutation in ISCU associated with mitochondrial myopathy". Journal of Medical Genetics. 54 (12): 815–824. doi:10.1136/jmedgenet-2017-104822. ISSN 1468-6244. PMC 5740555. PMID 29079705.
- ^ "#255125 - MYOPATHY WITH LACTIC ACIDOSIS, HEREDITARY; HML". www.omim.org. Retrieved 2023-11-24.
- ^ "#500002 - MITOCHONDRIAL MYOPATHY WITH DIABETES". www.omim.org. Retrieved 2023-11-24.
- ^ "DIABETES AND DEAFNESS, MATERNALLY INHERITED; MIDD - OMIM". www.omim.org. Retrieved 2024-03-02.
- ^ "#613076 - MYOPATHY, MITOCHONDRIAL PROGRESSIVE, WITH CONGENITAL CATARACT AND DEVELOPMENTAL DELAY; MPMCD". www.omim.org. Retrieved 2023-11-24.
- ^ "Phenotypic Series - PS600462 - Myopathy, lactic acidosis, and sideroblastic anemia (MLASA) - OMIM". www.omim.org. Retrieved 2023-11-30.
- ^ "Allelic Variants - 516060 - MT-ATP6 - OMIM". www.omim.org. Retrieved 2023-11-30.
- ^ "616209 - MYOPATHY, ISOLATED MITOCHONDRIAL, AUTOSOMAL DOMINANT; IMMD". www.omim.org. Retrieved 2023-11-30.
- ^ "#617675 - MYOPATHY, MITOCHONDRIAL, AND ATAXIA; MMYAT". www.omim.org. Retrieved 2023-11-30.
- ^ "#251900 - MITOCHONDRIAL MYOPATHY, EPISODIC, WITH OR WITHOUT OPTIC ATROPHY AND REVERSIBLE LEUKOENCEPHALOPATHY; MEOAL". www.omim.org. Retrieved 2023-11-30.
- ^ "#251950 - MITOCHONDRIAL MYOPATHY WITH LACTIC ACIDOSIS; MMLA". www.omim.org. Retrieved 2023-11-30.
- ^ "251945 - MITOCHONDRIAL MYOPATHY WITH A DEFECT IN MITOCHONDRIAL-PROTEIN TRANSPORT". www.omim.org. Retrieved 2023-11-30.
- ^ "*590000 - TRANSFER RNA, MITOCHONDRIAL, ALANINE; MTTA". www.omim.org. Retrieved 2023-11-30.
- ^ "*590015 - TRANSFER RNA, MITOCHONDRIAL, ASPARTIC ACID; MT-TD". www.omim.org. Retrieved 2023-11-30.
- ^ "Allelic Variants - 590095 - RANSFER RNA, MITOCHONDRIAL, TRYPTOPHAN; MT-TW - OMIM". www.omim.org. Retrieved 2023-11-30.
- ^ "Phenotypic Series - PS607426 - Coenzyme Q10 deficiency - OMIM". omim.org. Retrieved 2023-11-30.
- ^ "Phenotypic Series - PS252010 - Mitochondrial Complex I deficiency, nuclear type - OMIM". www.omim.org. Retrieved 2023-11-30.
- ^ "Phenotypic Series - PS252011 - mitochondrial complex II - OMIM". www.omim.org. Retrieved 2023-11-30.
- ^ "Allelic Variants - 516020 - cytochrome b of complex III - OMIM". www.omim.org. Retrieved 2023-11-30.
- ^ "Phenotypic Series - PS124000 - Mitochondrial complex III deficiency, nuclear type - OMIM". www.omim.org. Retrieved 2023-12-01.
- ^ "Phenotypic Series - PS220110 - Mitochondrial complex IV deficiency - OMIM". www.omim.org. Retrieved 2023-11-30.
- ^ "Phenotypic Series - PS604273 - Mitochondrial complex V deficiency - OMIM". www.omim.org. Retrieved 2023-12-01.
- ^ Straub V, Murphy A, Udd B (August 2018). "229th ENMC international workshop: Limb girdle muscular dystrophies - Nomenclature and reformed classification Naarden, the Netherlands, 17-19 March 2017". Neuromuscular Disorders. 28 (8): 702–710. doi:10.1016/j.nmd.2018.05.007. PMID 30055862. S2CID 51865029.
- ^ Bisceglia L, Zoccolella S, Torraco A, Piemontese MR, Dell'Aglio R, Amati A, et al. (June 2010). "A new locus on 3p23-p25 for an autosomal-dominant limb-girdle muscular dystrophy, LGMD1H". European Journal of Human Genetics. 18 (6): 636–641. doi:10.1038/ejhg.2009.235. PMC 2987336. PMID 20068593.
- ^ "613530 - MUSCULAR DYSTROPHY, LIMB-GIRDLE, TYPE 1H; LGMD1H". www.omim.org. Retrieved 2023-11-30.
- ^ Sanaker, Petter S.; Toompuu, Marina; Hogan, Vanessa E.; He, Langping; Tzoulis, Charalampos; Chrzanowska-Lightowlers, Zofia M. A.; Taylor, Robert W.; Bindoff, Laurence A. (2010-06-01). "Differences in RNA processing underlie the tissue specific phenotype of ISCU myopathy". Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease. 1802 (6): 539–544. doi:10.1016/j.bbadis.2010.02.010. ISSN 0925-4439.
- ^ Shaul, Orit (2017-10-01). "How introns enhance gene expression". The International Journal of Biochemistry & Cell Biology. Splicing. 91: 145–155. doi:10.1016/j.biocel.2017.06.016. ISSN 1357-2725.
- ^ "What is noncoding DNA?: MedlinePlus Genetics". medlineplus.gov. Retrieved 2024-04-11.
- ^ Moraes, C. T.; Shanske, S.; Tritschler, H. J.; Aprille, J. R.; Andreetta, F.; Bonilla, E.; Schon, E. A.; DiMauro, S. (March 1991). "mtDNA depletion with variable tissue expression: a novel genetic abnormality in mitochondrial diseases". American Journal of Human Genetics. 48 (3): 492–501. ISSN 0002-9297. PMC 1682992. PMID 1998336.
- ^ "#609560 - MITOCHONDRIAL DNA DEPLETION SYNDROME 2 (MYOPATHIC TYPE); MTDPS2". www.omim.org. Retrieved 2023-12-06.
- ^ a b "Ragged-red muscle fibers (Concept Id: C3275417) - MedGen - NCBI". www.ncbi.nlm.nih.gov. Retrieved 2023-12-06.
- ^ a b Rifai Z, Welle S, Kamp C, Thornton CA (January 1995). "Ragged red fibers in normal aging and inflammatory myopathy". Annals of Neurology. 37 (1): 24–29. doi:10.1002/ana.410370107. PMID 7818253. S2CID 23909958.
- ^ Gomes AP, Price NL, Ling AJ, Moslehi JJ, Montgomery MK, Rajman L, et al. (December 2013). "Declining NAD(+) induces a pseudohypoxic state disrupting nuclear-mitochondrial communication during aging". Cell. 155 (7): 1624–1638. doi:10.1016/j.cell.2013.11.037. PMC 4076149. PMID 24360282.
- ^ Kim JM (November 2017). "Myopathy, Drugs, and Mitochondria". Journal of Korean Medical Science. 32 (11): 1732–1733. doi:10.3346/jkms.2017.32.11.1732. PMC 5639049. PMID 28960021.
- ^ Coulter DL (2014-01-01). "Carnitine Deficiency". In Aminoff MJ, Daroff RB (eds.). Encyclopedia of the Neurological Sciences (Second ed.). Oxford: Academic Press. pp. 597–599. doi:10.1016/B978-0-12-385157-4.00079-8. ISBN 978-0-12-385158-1. Retrieved 2023-11-30.
- ^ Li Q, Yang C, Feng L, Zhao Y, Su Y, Liu H, et al. (2021). "Glutaric Acidemia, Pathogenesis and Nutritional Therapy". Frontiers in Nutrition. 8: 704984. doi:10.3389/fnut.2021.704984. PMC 8714794. PMID 34977106.
- ^ Béhin A, Acquaviva-Bourdain C, Souvannanorath S, Streichenberger N, Attarian S, Bassez G, et al. (March 2016). "Multiple acyl-CoA dehydrogenase deficiency (MADD) as a cause of late-onset treatable metabolic disease". Revue Neurologique. 172 (3): 231–241. doi:10.1016/j.neurol.2015.11.008. PMID 27038534.
- ^ Henriques BJ, Katrine Jentoft Olsen R, Gomes CM, Bross P (April 2021). "Electron transfer flavoprotein and its role in mitochondrial energy metabolism in health and disease". Gene. 776: 145407. doi:10.1016/j.gene.2021.145407. PMC 7949704. PMID 33450351.
- ^ "#616839 - EXERCISE INTOLERANCE, RIBOFLAVIN-RESPONSIVE; RREI". www.omim.org. Retrieved 2023-11-24.
- ^ Schoser, B. G. H.; Müller-Höcker, J.; Horvath, R.; Gempel, K.; Pongratz, D.; Lochmüller, H.; Müller-Felber, W. (October 2007). "Adult-onset glycogen storage disease type 2: clinico-pathological phenotype revisited". Neuropathology and Applied Neurobiology. 33 (5): 544–559. doi:10.1111/j.1365-2990.2007.00839.x. ISSN 0305-1846. PMID 17573812. S2CID 25822083.
- ^ a b c Saha, Madhurima; Reddy, Hemakumar M.; Salih, Mustafa A.; Estrella, Elicia; Jones, Michael D.; Mitsuhashi, Satomi; Cho, Kyung-Ah; Suzuki-Hatano, Silveli; Rizzo, Skylar A.; Hamad, Muddathir H.; Mukhtar, Maowia M.; Hamed, Ahlam A.; Elseed, Maha A.; Lek, Monkol; Valkanas, Elise (2018-11-01). "Impact of PYROXD1 deficiency on cellular respiration and correlations with genetic analyses of limb-girdle muscular dystrophy in Saudi Arabia and Sudan". Physiological Genomics. 50 (11): 929–939. doi:10.1152/physiolgenomics.00036.2018. ISSN 1531-2267. PMC 6293114. PMID 30345904.
- ^ Veerapandiyan A, Shashi V, Jiang YH, Gallentine WB, Schoch K, Smith EC (December 2010). "Pseudometabolic presentation of dystrophinopathy due to a missense mutation". Muscle & Nerve. 42 (6): 975–979. doi:10.1002/mus.21823. PMC 5506871. PMID 21104870.
- ^ Barton, Elisabeth R.; Pacak, Christina A.; Stoppel, Whitney L.; Kang, Peter B. (2020-07-29). "The ties that bind: functional clusters in limb-girdle muscular dystrophy". Skeletal Muscle. 10 (1): 22. doi:10.1186/s13395-020-00240-7. ISSN 2044-5040. PMC 7389686. PMID 32727611.
- ^ Sainio, Markus T.; Välipakka, Salla; Rinaldi, Bruno; Lapatto, Helena; Paetau, Anders; Ojanen, Simo; Brilhante, Virginia; Jokela, Manu; Huovinen, Sanna; Auranen, Mari; Palmio, Johanna; Friant, Sylvie; Ylikallio, Emil; Udd, Bjarne; Tyynismaa, Henna (February 2019). "Recessive PYROXD1 mutations cause adult-onset limb-girdle-type muscular dystrophy". Journal of Neurology. 266 (2): 353–360. doi:10.1007/s00415-018-9137-8. ISSN 1432-1459. PMC 6373352. PMID 30515627.
